Evaluating Stroke in the Acute Care Setting
Stroke Evaluation in the Acute Care Setting
Evaluating a patient who has experienced a stroke in the acute care setting is a complex process. As occupational therapists (OTs), our role is to assess various domains that affect patient function and quality of life. I have listed the top 10 key areas to focus on during the evaluation of patients diagnosed with stroke or presenting with stroke-like symptoms in the acute care setting.
1. Assess Motor Function
Motor evaluation begins with assessing the patient’s overall motor control and voluntary movement patterns during normal daily activities.
Areas that should be addressed include:
Functional ability of the arms and legs during engagement in ADLs
Self protection of the arm
Skin integrity
Tone and spasticity
OT assessment measuring tone: Modified Ashworth Scale
“The modified Ashworth scale is a muscle tone assessment scale used to assess the resistance experienced during passive range of motion, which does not require any instrumentation and is quick to perform” (Harb & Kishner, pgs. 358-359, 2023).
0: No increase in muscle tone
1: Slight increase in muscle tone, with a catch and release or minimal resistance at the end of the range of motion when an affected part(s) is moved in flexion or extension
1+: Slight increase in muscle tone, manifested as a catch, followed by minimal resistance through the remainder (less than half) of the range of motion
2: A marked increase in muscle tone throughout most of the range of motion, but affected part(s) are still easily moved
3: Considerable increase in muscle tone, passive movement difficult
4: Affected part(s) rigid in flexion or extension (Harb & Kishner, pgs. 358-359, 2023).
2. Assess Range of Motion
Joint mobility can be affected by both neurological and mechanical factors post-stroke. OTs should measure active and passive ROM in the affected and unaffected limbs, noting any limitations. Strength assessments, typically using manual muscle testing or handheld dynamometry, help gauge the muscle’s capacity to perform functional tasks.
Assess proximal/ distal range of motion because they often return at different rates.
Range of motion should be documented in terms of 0, 1/4, 1/2, 3/4, and full versus ACTUAL degrees.
To improve shoulder ROM, support the hemiplegic or weak arm by holding the humerus approximately 4 inches away from the axialla while maintaining ER with the thumb pointing up towards the ceiling (Smith-Gabai & Holm, p. 360, 2017).
Do NOT test strength on a patient with stroke/ neurological deficits unless the movement appears to be normal.
3. Ask Pain
In individuals diagnosed with stroke, approximately 11% of patients will develop chronic pain for various reasons (e.g., central, subluxation, spasticity, etc) (Smith-Gabai & Holm, p. 360, 2017).
Always assess pain when you are evaluating a patient and ask the location as well as a description of the pain.
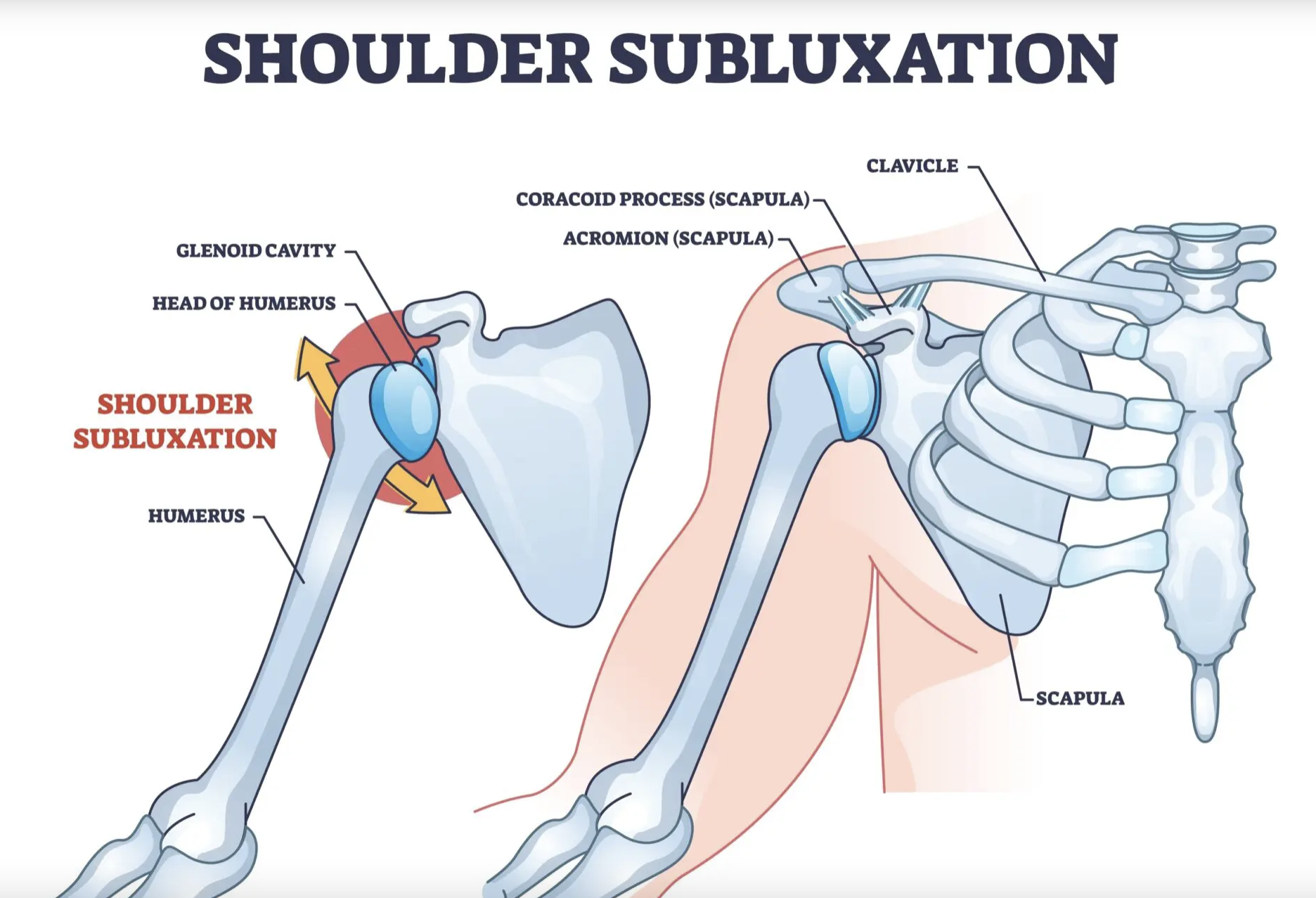
4. Assess for a Shoulder Subluxation
Shoulder subluxation, common post-stroke, requires careful assessment. Observing the patient's posture and palpating the shoulder complex can help identify any displacement of the humeral head. Early intervention strategies, including education on positioning and potential use of slings or supports, can reduce complications associated with subluxation.
To test for subluxation, you use the finger-breadth palpation method used for quantifying the size of the subluxation.
Teach the patient’s family proper positioning and precautions. Post written instructions in the patient’s room with pictures to illustrate the arm supported in bed, and when sitting up in a chair (Smith-Gabai & Holm, p. 361, 2017).
Click this link for an explanation of shoulder subluxation and ways to manage symptoms following a stroke. I am not affiliated with Post Stroke on Youtube. I have provided this link for educational purposes only. The video was created by Elyse Newland, an Occupational Therapist.
Image retrieved from ProHealthClinic, 2023
5. Range of Motion Precautions
Specific precautions regarding range of motion should be established based on the individual patient's condition. For example, individuals with significant hemiparesis may have contraindications related to shoulder ROM.
The following information retrieved from (Smith-Gabai & Holm, p. 361, 2017):
The patient must have at least 45 degrees of external rotation with the shoulder fully abducted before evaluating the arm.
The shoulder should not be passively moved beyond 90 degrees of flexion and abduction unless the scapula is upwardly rotated and the humerus is externally rotated.
External rotation to 45 degrees becomes the primary issue with the emergence of flexor synergistic patterning. Without 45 degrees of external rotation the patient will not be able to lift the arm. Limitation in external rotation, have been shown to be a high predictor of developing hemiplegic shoulder pain.
Do not use pulleys with unstable, weak, or flaccid shoulders. They will contibute to shoulder tissue injury becuase the shoulder typically is not properly aligned, nor does it have the stabilizing capability for proper kinematics.
PROM training for families should include instruction of no PROM past 90 degrees so as to minimize painful pathologies as synergistic patterning emerges. Families will need education on proper PROM to avoid extreme flexion or abduction of the hemiplegic UE. Maintaining ER at least 45 degrees is imperative for long-term recovery. If time is available for only exercise or stretch choose external rotation.
6. Utilize Principles of Neuroplasticity
In evaluating cognitive functioning, it's essential to understand the principles of neuroplasticity, which underline the brain’s capacity to reorganize and adapt following injury. OTs should assess the patient's previous engagement in therapeutic activities and their current capacity to participate in interventions that stimulate neuroplastic changes.
Educate the patient and caregiver about how changes in the brain and motor recovery occur even in the early stages of acute rehab.
Examples of interventions to encourage neuroplastiticy include:
Using the affected hand to perform part of a sponge bath.
Self-feeding finger foods.
Sitting on the edge of the bed to increase alterness.
Encourage the caregivers to stand on the affected side to encourage visual attention (Smith-Gabai & Holm, p. 361, 2017).
Weight-bearing activities on the affected upper extremity.
7. Evaluate Sensation
Sensation should be comprehensively evaluated given its role in motor recovery and functional independence.
For a low-level patient who is minimally concsious or comatose, pain assessment can be performed using nail bed pressure, tugging or pinching the ear or arm, or a sternal rub.
A screening method to asses proprioception:
Have the patient flex both shoulders to 90 degrees, close their eyes, and name 5 states. If the patient’s affected arm drifts ask them if their arm is still in the same place. If the answer is yes, then proprioception is likely impaired (Smith-Gabai & Holm, p. 361, 2017).
8. Utilize Splinting
The use of splints can be beneficial in maintaining optimal positioning, facilitating movement, and preventing contractures. OTs should assess the need for custom or pre-fabricated splints based on the patient's specific limitations and goals.
Reasons that necessitate a splint include increasing tone with the fingers flexed so tightly that palmar skin integrity is at risk, edema, fracture, or nerve palsy.
If a splint is necessary, consider using a volar-based resting mitt splint with the wrist in neutral or slightly extended position, fingers minimally flexed and the thumb abducted. This allows for a reflex-inhibiting posture for flexor synergistic tone and can be modified later as needed (Smith-Gabai & Holm, p. 363, 2017).
Consider wearing splint wear for nighttime with limited day time wear (at most 4 hours). Coordinate the splint wear schedule to meet the needs of the patient and the nursing staff. This schedule allows nurses time to put on and take off the splint when they are doing their initial assessments at shift change and during neuro checks every 4 hours (Smith-Gabai & Holm, p. 363, 2017).
9. Assess Cognition
A thorough cognitive assessment is essential for understanding the patient’s readiness to participate in rehabilitation. Evaluating levels of consciousness, attention, memory, executive function, and direction following can help OT’s tailor interventions appropriately. Typically in the acute care setting, cognition is evaluated through functional task performance (participation in ADLs) (Smith-Gabai & Holm, p. 363, 2017). Most often, it is important to ask orientation questions: person, place, time, situation.
Person: “Can you confirm your name and date of birth?”
Time: “What year is it?”
Place: “What State are you in?” “Where are you right now?”
Situation: “Can you tell me why you are in the hospital?”
10. Assess Safety/ Judgment
Lastly, assessing the patient’s safety judgment is crucial, particularly when planning for discharge. Evaluating their insight into their condition, decision-making skills, and ability to follow through with safety measures is essential prior to discharge.
The evaluation of stroke patients in the acute care setting is multifaceted, requiring OTs to gather comprehensive information across multiple domains. By addressing motor function, sensation, cognition, and safety considerations, we can create individualized rehabilitation plans that promote optimal recovery outcomes. Effective evaluations not only help inform immediate care but also lay the foundation for continued rehabilitation as patients progress in their recovery journey!
Please let me know if you have any questions in the comments below or email me at juliannemadeline.ot@gmail.com
References
Harb, A., Kishner, S. (2023). Modified Ashworth Scale. National Library of Medicine. https://www.ncbi.nlm.nih.gov/books/NBK554572/#:~:text=The%20modified%20Ashworth%20scale%20is%20a%20muscle%20tone%20assessment%20scale,and%20is%20quick%20to%20perform.
Smith-Gabai, H & Holm, S. (2017). Occupational Therapy in Acute Care 2nd Ed. AOTA Press.